Mental health during pregnancy and in the postnatal period
During pregnancy and after the birth of a child, women are at a higher risk of experiencing mental health problems. This period is also a time when a range of mental health conditions that a woman may have previously experienced can return or worsen. Low mood, anxiety and depression are common mental health problems that occur during pregnancy and in the year after childbirth.
Perinatal mental health conditions are wide-ranging, and can include:
- Low mood – feeling sad, mood swings or crying episodes
- Depression – persistent sadness, lack of pleasure in things that normally bring joy, feelings of inadequacy or guilt, thoughts of death or suicide
- Anxiety, obsessive thoughts or post-traumatic stress – excessive worry, obsessions or persistent intrusive thoughts, compulsions or repetitive behaviours that are difficult to control, flashbacks or nightmares, intrusive re-experiencing of a traumatic experience
- Psychosis – delusions or strange beliefs, hallucinations, hyperactivity, paranoia, rapid mood swings.
Mind Cymru say around 30% of parents suffer anxiety or depression in the first year after their baby's birth. In 2016, the Mental Health Foundation published ‘Mental Health in Wales: Fundamental Facts 2016’. In that report, they state that mental health problems affect more than 1 in 10 women during pregnancy and the first year after childbirth.
Maternal Mental Health – Women’s Voices
In February 2017, the Royal College of Obstetricians and Gynaecologists published a report ‘Maternal Mental Health – Women’s Voices’. The UK report describes women's experiences of perinatal mental health problems, based on a survey of over 2,300 women from across the UK who had given birth in the last five years. By surveying women, the College aimed to understand the current provision of perinatal mental health care to identify gaps, to provide better training where necessary and to advocate for change. Just over 3 per cent (59 responses) were from women living in Wales.
In their written evidence to the Children, Young People and Education Committee as part of its Perinatal Mental Health Inquiry, the Royal College of Obstetricians and Gynaecologists summarised their survey findings from the Welsh cohort.
The Royal College’s survey found that in Wales, 91% of women who responded experienced at least one perinatal mental health condition, with 82% experiencing low mood, 59% experiencing anxiety and 55% experiencing depression. The survey found:
- In Wales, 26% of women were not asked by any healthcare professional during or after their pregnancy about their mental well-being, compared with a national UK average of 15%.
- In Wales, 20% of respondents said that they did not talk to, or would not have felt comfortable talking to any healthcare professionals about their mental wellbeing during or after pregnancy, compared with 16% nationally.
- Women in Wales said they would have felt most comfortable talking about how they were feeling with their midwife.
- The most common reasons for respondents to the survey not feeling comfortable, or not talking to a healthcare professional about their mental wellbeing was that they were concerned about it being noted in their medical records.
- Of those women who experienced symptoms, getting a referral to further services was often very difficult, with little support or signposting to services. In Wales, 22% reported being referred, with 54% having no further information about where to seek help.
- In Wales, 58% of respondents reported waiting over four weeks after referral to be seen, compared to 38% across the whole of the UK.
The UK report presents a stark picture of an NHS in which women with poor maternal mental health during pregnancy and after birth experience low rates of onward referral and long waits, with many seeking private treatment as a result.
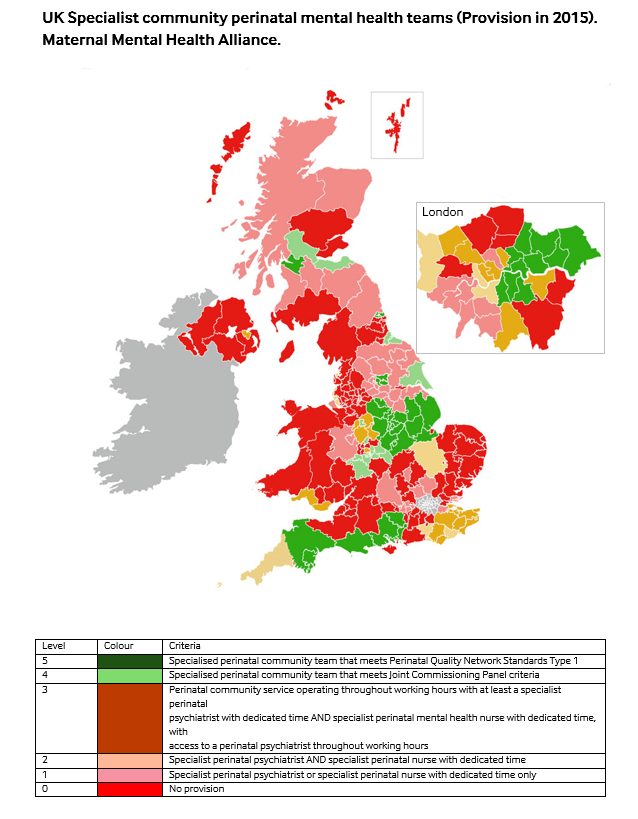
The following map was produced by the Maternal Mental Health Alliance for their Everyone's Business Campaign in 2015. It shows what the provision of specialist community perinatal mental health services was in the UK in 2015.
In Wales (as in England), additional funding has been provided to improve specialist care. In 2015, the Welsh Government announced an extra £1.5million in funding to improve outcomes for women with perinatal illnesses.
There are no mother and baby units in Wales, following the closure of the mother and baby unit at the University Hospital of Wales in Cardiff in 2013.
The Children, Young People and Education Committee’s Inquiry on Perinatal Mental Health (see previous blog article), will provide a uniquely Welsh perspective on the services needed across Wales, and the extent to which women in Wales can access the specialist care they need.
The Committee will be hearing directly from women and their families about their experiences next week (Thursday 18 May). This will be followed by a number of oral evidence sessions from key stakeholders starting on 24 May 2017 (see Children, Young People and Education Committee webpages for more information).
Article by Sarah Hatherley, National Assembly for Wales Research Service.
Image source: everyonesbusiness.org.uk
This post is also available as a print-friendly PDF: “The pain these conditions cause women and their families is significant”. The Royal College of Obstetricians and Gynaecologists describe the impact of perinatal mental health problems on women and their families. (PDF, 281KB)