New data reinforces concerns expressed by public health experts that vaccine uptake is lower among some ethnic groups and in deprived areas.
In March Public Health Wales (PHW) published its second monthly report on inequalities in vaccination uptake, which provides a breakdown of vaccinations by priority group, age, sex, ethnicity and deprivation.
Our article on vaccination data outlines who has received a first and second dose of a vaccine by priority group across Wales and by Local Health Boards.
Who’s still at risk?
The Scientific Advisory Group for Emergencies (SAGE) ethnicity sub-group raised concerns in December 2020 of “a significant risk” that vaccine uptake for COVID-19 will be lower among some ethnic groups, based on levels of uptake from previous vaccination programmes.
Similar views were expressed by the King’s Fund who warned of a “risk the vaccination programme will further entrench the inequalities that have been so brutally exposed by the pandemic”.
The Welsh Government published an updated vaccine strategy in February which says it has “reached out to and engaged with a wide range of communities, partners and stakeholders” to “[ensure] no one is left behind”.
In February the Health Minister, Vaughan Gething, and Deputy Minister and Chief Whip, Jane Hutt, issued a statement urging everyone to take up the vaccine. It noted that the Welsh Government was working with race and faith groups, and considering using mosques and other places of worship for vaccinations.
However, the data shows that some groups of people have a lower than average vaccine uptake, and PHW highlights the “significant inequalities in coverage of COVID-19 vaccine in Wales”.
The biggest cause for concern is that the same groups with lower levels of uptake of the vaccine are the ones who are at a higher risk of death from COVID-19.
People from some ethnic groups
PHW’s report highlights that the largest inequality is that 75.3% of those aged 65-69 from Black, Asian, Mixed and Other ethnic groups combined received a vaccine, compared to 88.6% in the White ethnic group aged 65-69.
Uptake of at least one dose of a COVID-19 vaccine by age and ethnic group
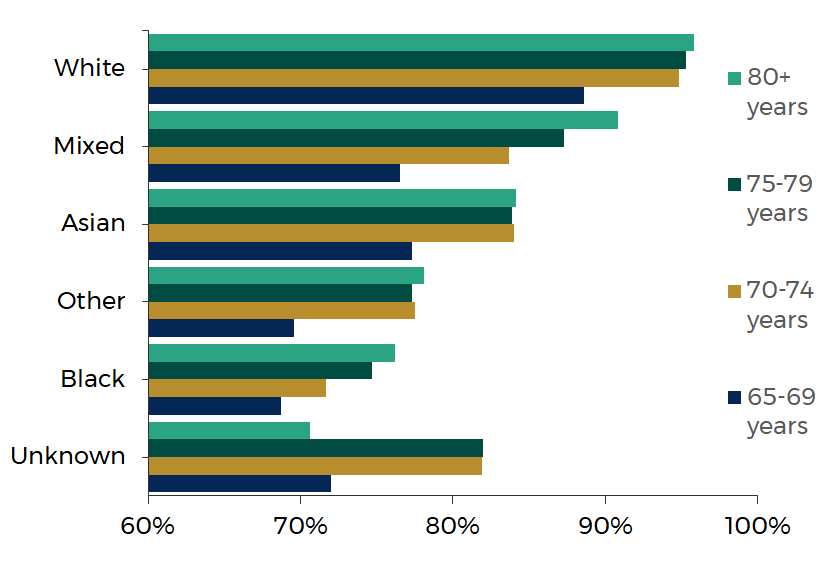
Source: Public Health Wales
The graph above shows that people from the Black ethnic group have the lowest level of uptake compared to the other reported ethnic groups in all age groups (except those whose ethnic group is unknown).
In the summer, the Office for National Statistics (ONS) reported that males from the Black ethnic background had the highest death rate from COVID-19. It found that males from the Black African ethnic background had a 2.7 times higher death rate compared to males from the White ethnic background.
Death rates involving COVID-19 by ethnic group, aged 9 to 110 years of age in England and Wales

Source: Office for National Statistics
As shown in the graph above, males of Black African, Bangladeshi and Black Caribbean ethnic background had the highest rates of death, significantly higher than all other ethnic groups.
People living in the most deprived areas
The graph below shows uptake by age group and areas of deprivation measured by the Welsh Index of Multiple Deprivation (WIMD). WIMD is an overall measure of deprivation based on a number of factors such as income, employment, health and education.
Uptake of at least one dose of a COVID-19 vaccine by age and Welsh Index of Multiple Deprivation quintile
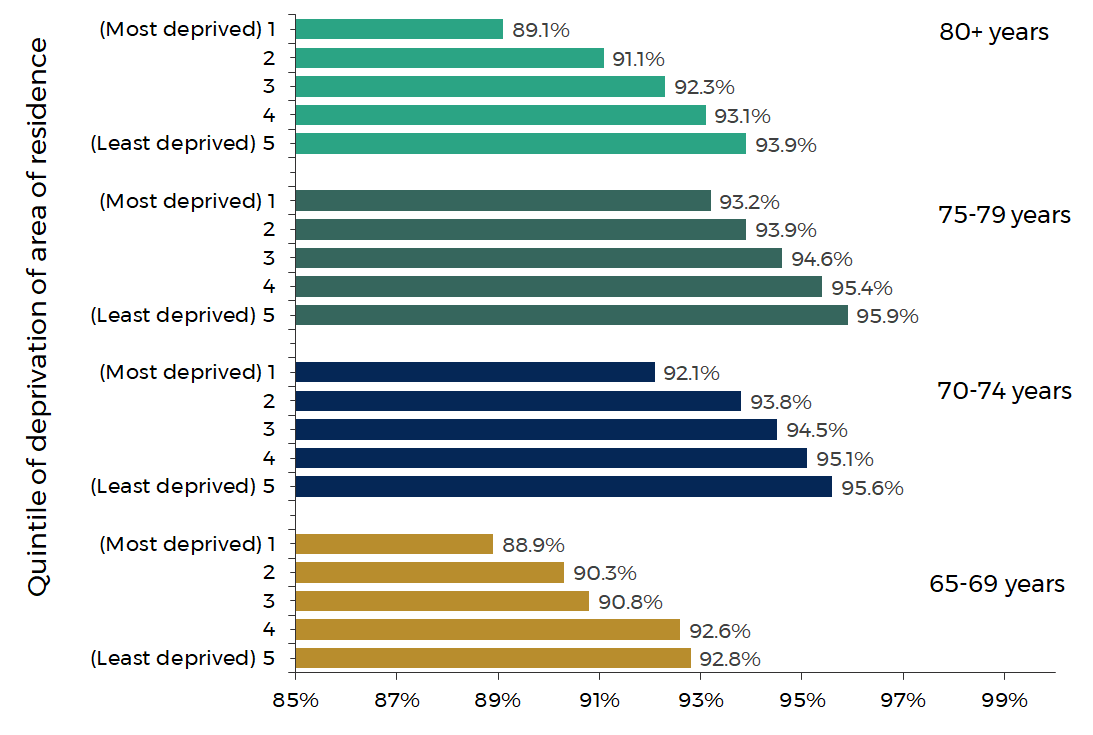
Source: Public Health Wales
In each age group shown there is a stark difference in the uptake of a vaccine between the most and least deprived areas. The largest difference in uptake is seen in those aged 80 and over at 4.8 percentage points.
The graph below shows that the mortality rate from COVID-19 in the most deprived areas was nearly twice as high as that in the least deprived areas.
Age standardised mortality rates of all deaths involving COVID-19 by Welsh Index of Multiple Deprivation
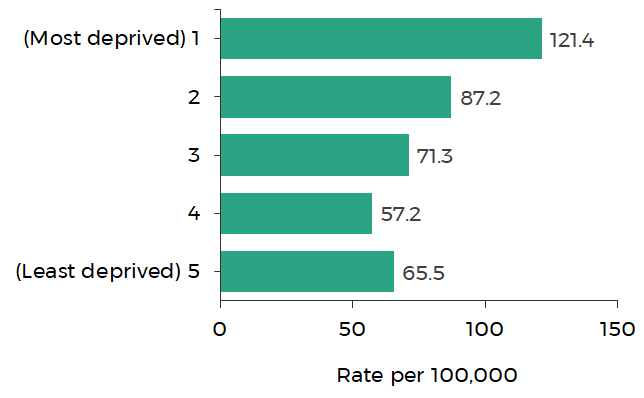
Source: Office for National Statistics
Note: The graph shows deaths occurring between 1 March 2020 and 31 July 2020 and registered by 15 August 2020.
What does this mean?
Wales is starting to ease the restrictions currently in place to control the virus. The modelling to predict the impact of easing restrictions, and thereby increasing mixing between people, suggests a third wave of the pandemic is likely in most scenarios.
A resurgence of the virus is likely because many people do not have protection from COVID-19. Either because they haven’t been vaccinated or because their vaccine won’t prevent all infection or illness (even though they’re highly effective, the vaccines don’t provide perfect protection).
This means that communities where uptake is lower will be particularly at risk from an increase in the spread of COVID-19.
Why are some people reluctant to get vaccinated?
A recent ONS survey found that Black or Black British adults had the highest level of vaccine hesitancy compared to other ethnic groups. 44% of Black or Black British adults reported vaccine hesitancy compared to 8% of White adults.
Reported vaccine hesitancy by ethnic group
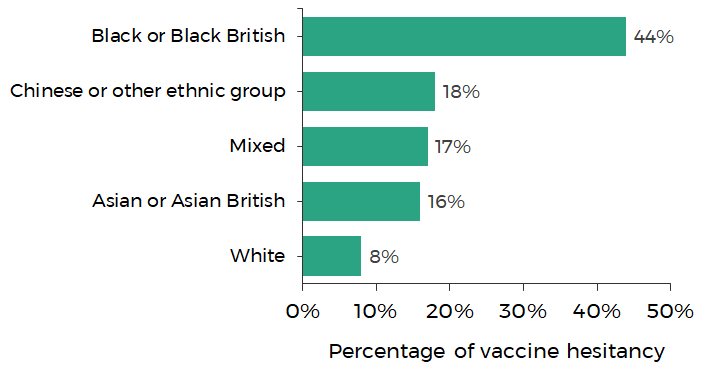
Source: Office for National Statistics
In a survey carried out by PHW in March, reasons given for not wanting to receive a vaccine included:
- not trusting the vaccines due to the speed of their development and unknown side effects;
- having heard about adverse reactions to the vaccines;
- not feeling a need to be vaccinated; and
- being suspicious towards the vaccination process.
Results from ONS surveys show similar reasons being raised. The graph below shows the five most common reasons for not wanting to take a vaccine.
Reasons for not taking a vaccine for COVID-19 if/when it is offered
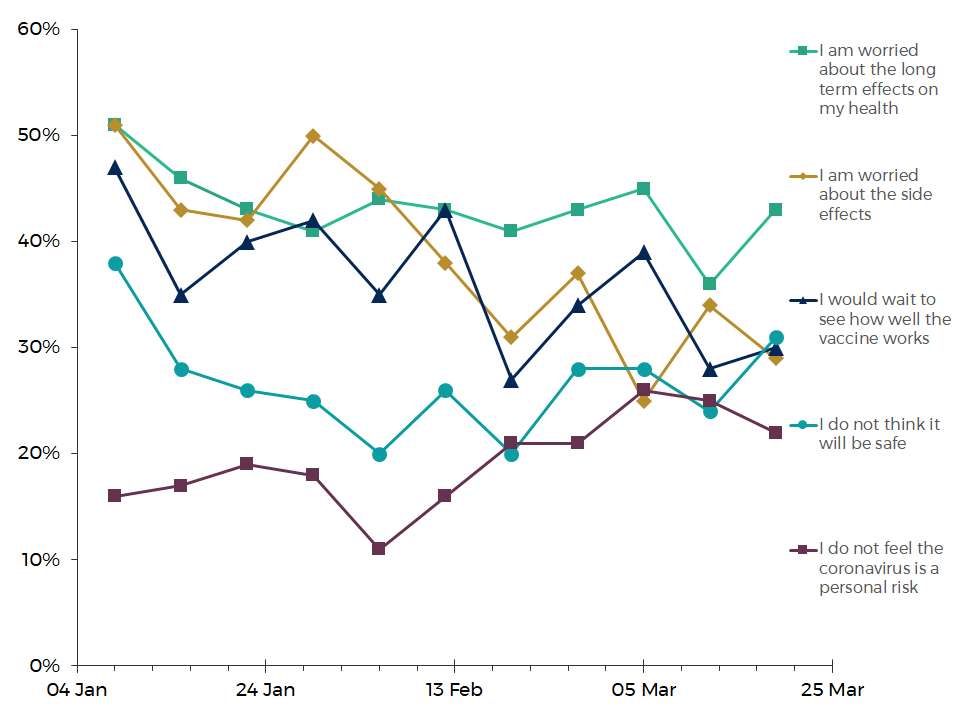
Source: Office for National Statistics
43% of respondents who were fairly or unlikely to have a vaccine if offered said they were worried about the long term effects on their health. This has been the most common reason since mid-February 2021.
Research by SAGE’s ethnicity sub-group suggests that specific reasons for vaccine hesitancy among some ethnic groups include:
- low confidence in the vaccine;
- perception of risk;
- distrust of public authorities;
- inconvenience and access barriers;
- socio-demographic context and lack of endorsement, and
- lack of vaccine offer or lack of communication from trusted providers and community leaders.
What can be done to overcome vaccine hesitancy?
Some suggested solutions from SAGE’s ethnicity sub-group to overcoming these barriers include:
- improving trust through GPs and health centres by recommending and offering vaccines, and improving uptake among healthcare workers from all ethnic groups;
- community engagement, including working with community leaders, providing educational videos in different languages, and clear information on side effects;
- addressing access and convenience issues at a local level, for example by providing vaccinations in workplaces, community centres, and religious venues, providing support for booking appointments (including transport), and giving reminders for appointments; and
- culturally tailored communication shared by trusted sources, including training for healthcare staff to enable conversations about vaccine beliefs, and training for faith leaders on vaccine research.
In March the Welsh Government published a vaccination equity strategy which sets out that a new Vaccine Equity Committee will “ensure the equitable delivery of the vaccination programme”. The Committee will focus on four areas:
- Identifying areas for action: population groups with lower levels of uptake will be identified with local teams being encouraged to develop a understanding of local communities.
- Taking a community led approach: specific concerns and barriers to vaccination will be identified and local teams can provide insights into where effective interventions should be targeted.
- Tailoring messages: community led co-production of messages to help answer the fears and concerns that people have with the messages coming from local role models that reflect diversity.
- Accounting for diversity: consideration of the whole vaccination process to ensure reasonable adjustments can be made for individual needs.
The biggest worry is that the same groups with lower levels of uptake of the vaccine are the ones who are at a higher risk of death from COVID-19. These people will be at an increased risk if there’s a third wave of the virus. This presents a significant challenge in managing the impact of the virus on some of the most vulnerable people in Wales.
Article by Lucy Morgan, Senedd Research, Welsh Parliament






