Following the COVID-19 pandemic, patients are waiting longer for NHS care and planned operations. At the end of March 2023, there were approximately 734,700 patient pathways in Wales waiting to start hospital treatment.
The Senedd’s Health and Social Care Committee continues to monitor performance against the Welsh Government’s planned care recovery targets. It considered its third NHS waiting times monitoring report earlier this week.
This article looks at the decision to exclude some specialties from those recovery targets and what that means for the thousands of patients still waiting for NHS treatment.
Seven specialties are excluded from the targets for being “exceptionally challenging”
The Welsh Government’s recovery target to eliminate two year waits in most specialties by March 2023 doesn’t include seven specialties recognised as “exceptionally challenging”. The Welsh Government says these specialties had large numbers waiting prior to the COVID-19 pandemic.
The seven specialties are dermatology, general surgery, ophthalmology, urology, gynaecology, trauma and orthopaedics, and ear, nose and throat.
Figure 1: Number of patient pathways waiting longer than two years to start treatment in the specialities excluded from the Welsh Government’s recovery target
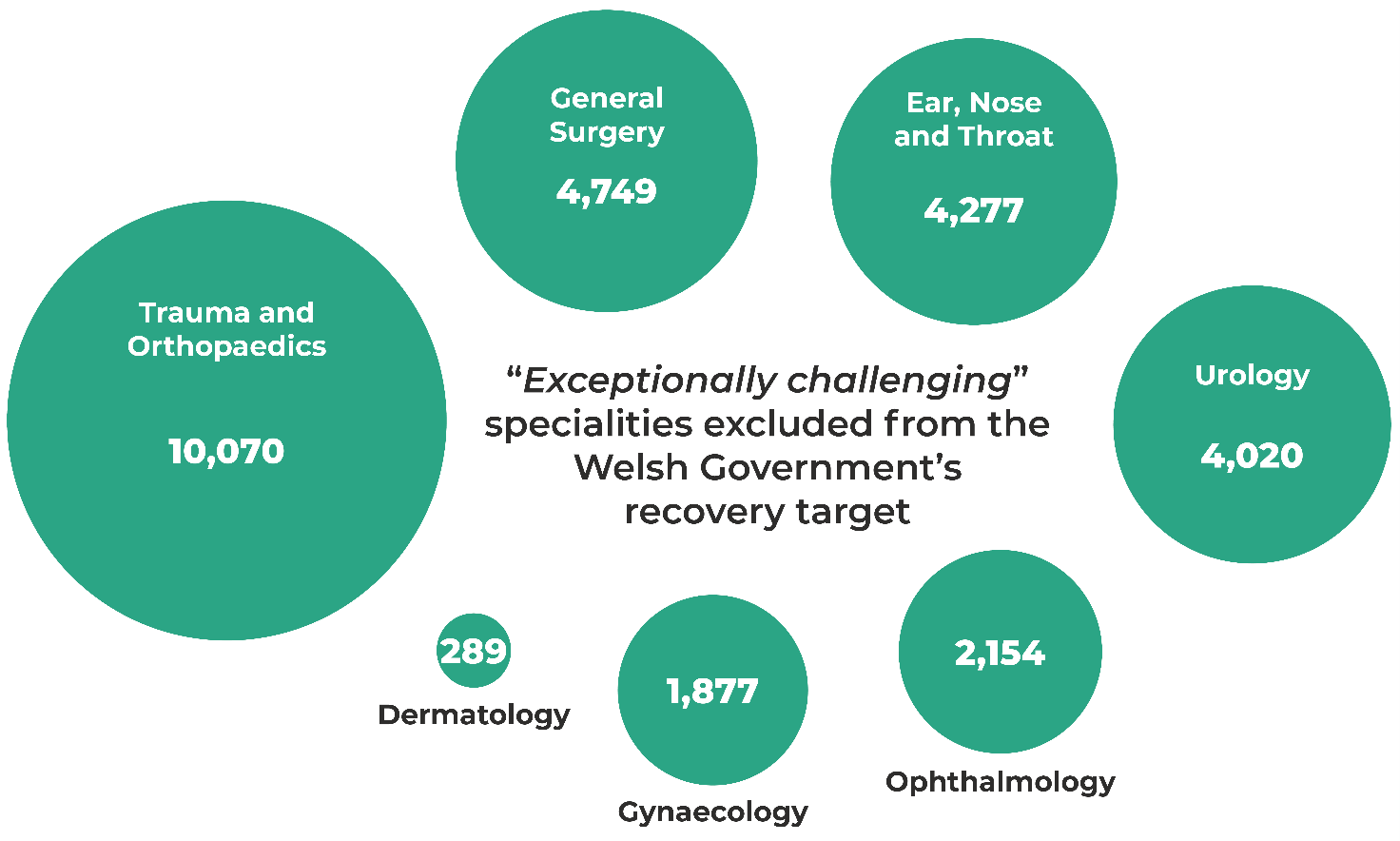
Patients waiting for trauma and orthopaedic care (which includes knee and hip replacements) are waiting the longest for NHS treatment. There were 31,349 patient pathways in Wales waiting over a year to be treated at the end of March for trauma and orthopaedics – around 10,070 of them had been waiting for more than two years.
Trauma and orthopaedics account for nearly a third (31.7%) of the total volume of patient pathways waiting more than two years for treatment.
Audit Wales published its report Orthopaedic Services in Wales – Tackling the Waiting List Backlog in March 2023. They found that urgent and sustainable action is needed to tackle the long orthopaedic waiting times and it could take three years or more to return the orthopaedic waiting list to pre-pandemic levels.
The Minister for Health and Social Services, Eluned Morgan, has said these ‘challenging specialties’ will be prioritised for action in 2023/24:
We are refocusing the national clinical groups in the planned care programme to provide leadership and challenge to share good practice and support the implementation of new ways of working to transform service delivery and drive down waits in these areas.
Progress on reducing NHS waits is slow across NHS services
The seven specialties outside the scope of the Welsh Government’s planned care recovery targets account for 86% (27,400) of the patient pathways waiting more than two years for NHS treatment.
On top of the seven ‘exceptionally challenging’ specialties, there were a further 17 specialties with patient pathways waiting more than two years in March 2023.
In addition to this, 52,925 patient pathways are waiting more than a year for their first outpatient appointment (i.e. patients with ailments waiting to be assessed before it is decided if they need hospital treatment).
The impact of NHS waiting times on patients
The Health and Social Care Committee commissioned a series of interviews and focus groups with people waiting for NHS treatment as part of an inquiry in 2022.
The Committee heard from an 83-year-old man with hip problems who was referred quickly by his GP to see a consultant and put on the NHS waiting list in early 2019. He was offered a steroid injection on two separate occasions to help ease the pain, but he refused because his surgeon told him: “your place in the queue will be rock bottom as the health board will deem it as you have been seen to”.
The hospital told him in early 2021, that he’d been moved from the routine to the urgent list. At the time of the Committee’s inquiry, he’d heard no more from the NHS. He’d been left waiting in pain, with a poorer quality of life, poor mental health, and an overall lack of confidence. He said:
I have to say that since Christmas, my hopes and aspirations have taken a nosedive. I know my condition has deteriorated; I now have to walk across the house with a walking stick. The pain is constant and getting to the point where even making a cup of tea is a physical and mental effort.
The Committee also heard from a 28-year-old woman who was diagnosed with endometriosis at 17 years. She’d paid privately to see a gynaecologist as she was experiencing bowel symptoms and wanted a scan.
She was then diagnosed with endometriosis on the bowel and was added to the NHS waiting list (she couldn’t afford to pay privately for the surgery). She was told the waiting list was six and a half years. She said she had very little pain management support, was left taking strong painkillers and:
I try my best and I feel so lucky to have such a supportive partner and family who really do understand. But I still feel a lot of guilt, I often wonder if I could be a better parent for her [my 4 year old daughter] because I can't go to the park with her. I can't take her out on walks and things because I'm in so much pain majority of the time. I just feel that she misses out on things that she shouldn’t be missing out on.
There is no doubt NHS Wales still faces significant pressures, and the latest figures are another reminder that all parts of the NHS are struggling.
Behind these statistics are patients waiting in pain or experiencing disruption to their daily lives, and that’s why the Health and Social Care Committee continues to monitor progress in tackling the NHS waiting list backlog: NHS Waiting Times Termly Monitoring Report (June 2023).
Article by Sarah Hatherley, Senedd Research, Welsh Parliament






