This article is part of our 'What's next? Key issues for the Sixth Senedd' collection.
The COVID-19 pandemic has put enormous pressure on health services, with lengthening waiting times for treatment. What can be done to tackle the backlog?
In March 2020 all non-urgent hospital treatments were postponed, freeing up hospital capacity to deal with the first wave of the COVID-19 pandemic. COVID-19 pressures are now easing, but NHS Wales is facing a sizeable backlog. Over half a million patients are currently waiting for treatment for other conditions. How can our healthcare services respond to this challenge?
What’s the scale of the challenge?
The Welsh Government’s targets for referral to treatment (RTT) are that 95% of patients referred for planned hospital treatment should be seen within 26 weeks, and 100% within 36 weeks. The RTT time also includes time waiting for out-patient appointments, tests, scans or other procedures that may be needed before being treated. There are other waiting times targets for diagnostic tests, therapies, and starting cancer treatment.
Waiting times were already increasing before the pandemic. At their most recent lowest point, in March 2019, the RTT total stood at 8,985 patients waiting over 36 weeks. But those numbers increased again over following months to 25,549 in December 2019. Between February 2020 and February 2021, total numbers waiting to start treatment rose from 461,809 to 549,353, with those waiting over 36 weeks growing from 25,634 to 217,655 patients – a 749% increase.
A fall in the numbers of patients being referred by GPs for treatment means there are fewer patients waiting under 36 weeks, but patients who were already on waiting lists are waiting longer. Around 60% of those waiting over 36 weeks are waiting for a first out-patient appointment.
Performance against Referral to Treatment (RTT) waiting times targets: Wales, February 2020-February 2021
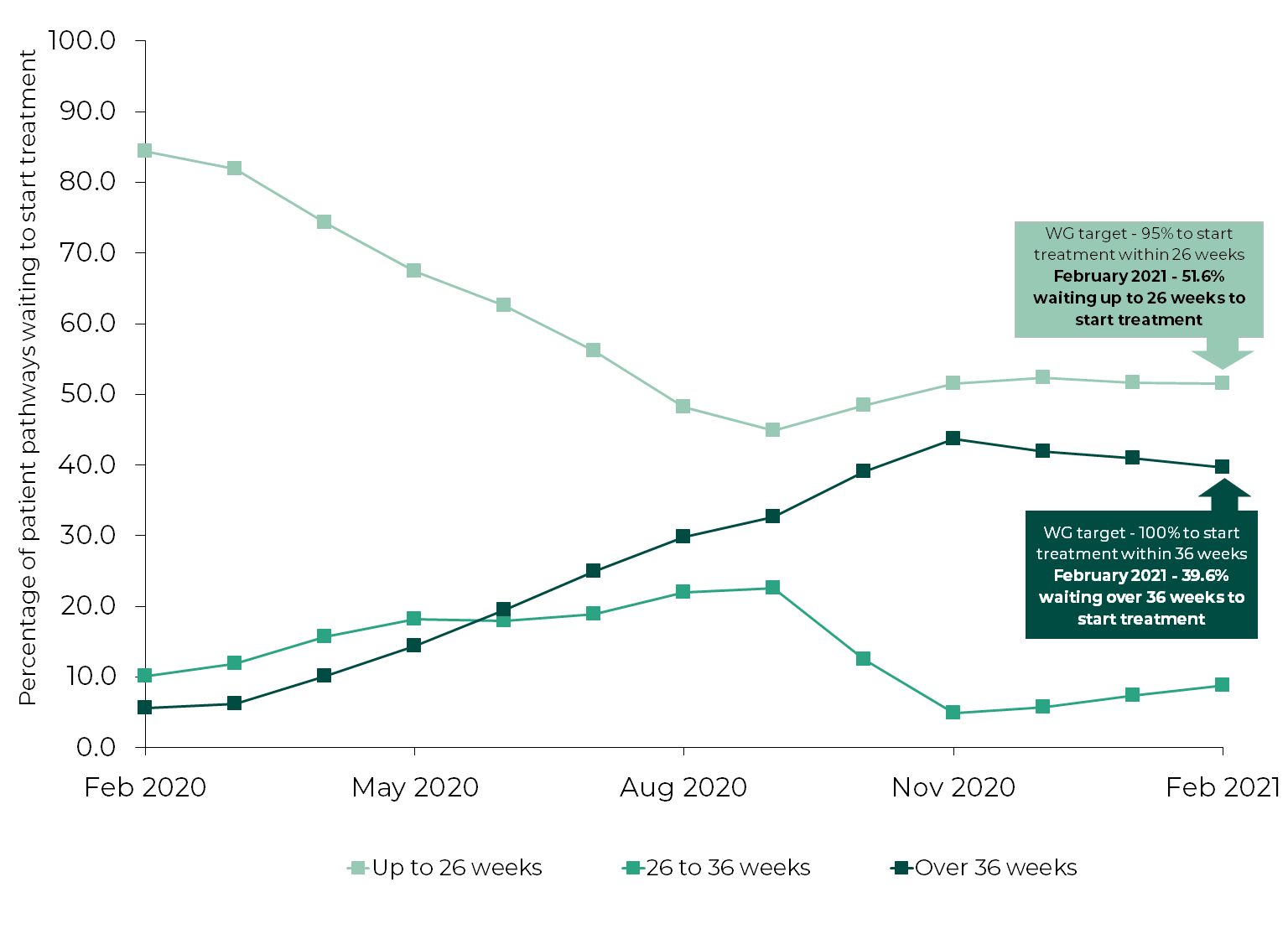
Source: StatsWales NHS Wales Hospital Waiting Times Referral to treatment
There are also Welsh Government targets stating that no-one should wait longer than eight weeks for diagnostic services, such as X-Rays, or 14 weeks for therapy services, such as physiotherapy. Between February 2020 and February 2021, the numbers waiting beyond these targets rose from 3,551 to 48,136 in diagnostics, and from 197 to 4,129 in therapies.
Percentage of patients waiting longer than diagnostic and therapy waiting times targets: Wales, February 2020-February 2021
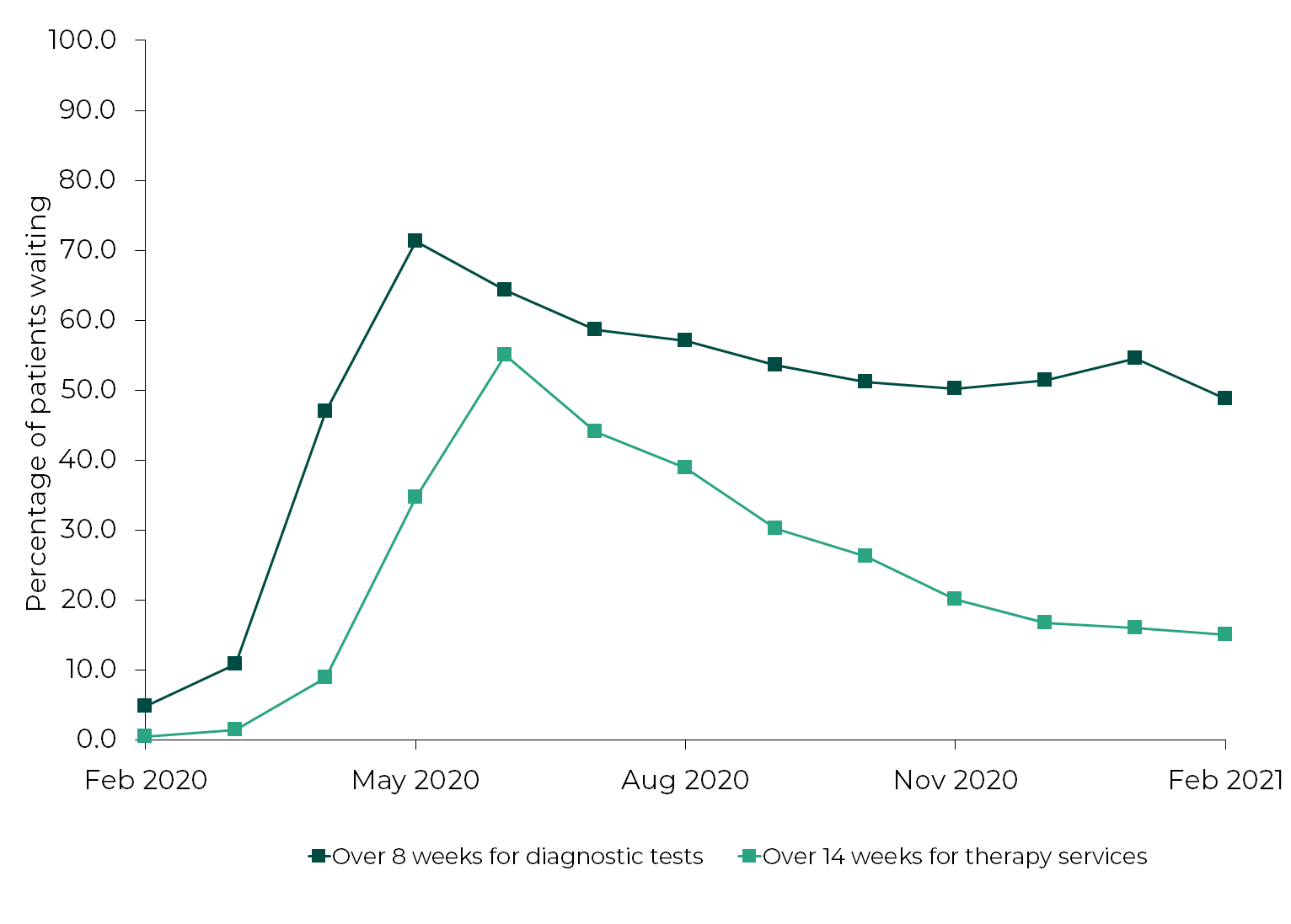
Source: StatsWales, NHS Wales Hospital Waiting Times Diagnostic and Therapy Services
Where are the key pressures?
The original decision to postpone non-urgent treatment applied across Wales. But since December 2020, health boards have been able to decide locally when and how much non-urgent work they could resume. Over time, this may mean the speed of dealing with the backlog varies across Wales. In December 2020, health boards were delivering only around half of the pre-pandemic levels of non-urgent activity.
Numbers of Referral to Treatment (RTT) patients waiting over 36 weeks by health board, February 2020 and February 2021
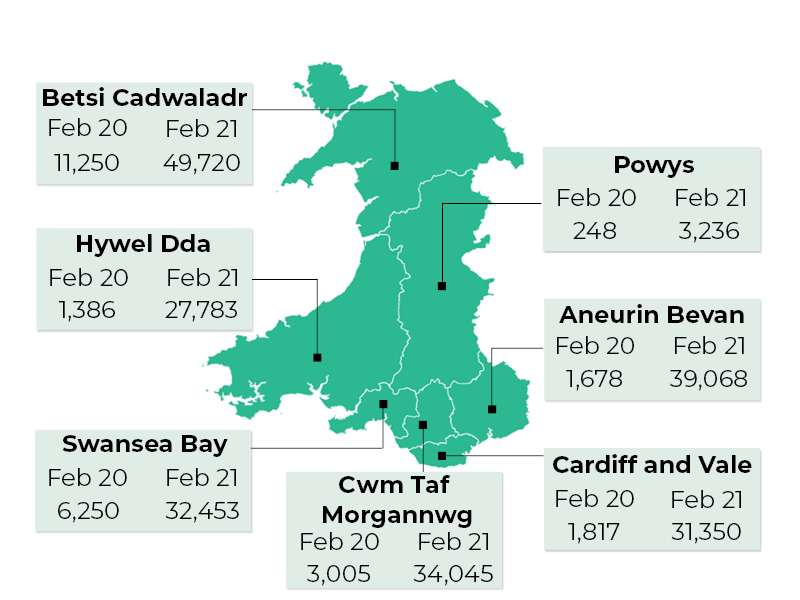
Source: StatsWales, NHS Wales Hospital Waiting Times Referral to treatment
Much of the growth in waiting lists comes from high-volume procedures for specific conditions, such as hip and knee replacements, or cataracts. Of the 217,655 patients waiting over 36 weeks, the majority are in a small number of specialties, including 52,173 in orthopaedics, 31,695 in ophthalmology, 26,354 in ear, nose and throat, 25,181 in general surgery, and 12,715 in dermatology.
Is that the whole picture?
The published figures tell only part of the story. GPs have made fewer referrals for treatment. Total monthly referrals fell from 109,432 in February 2020 to 39,103 in April 2020, and were only 82,647 in February 2021. The Fifth Senedd’s Health, Social Care and Sport (HSCS) Committee inquiry into the impact of COVID-19 on health and social care heard concerns around potential “pent-up demand”, including people with existing chronic conditions who needed ongoing support and assessment. Cardiff and the Vale UHB stated that:
For most services the lack of referrals is unlikely to reflect a change in the true health needs of the population - more likely the demand has simply been supressed by the pandemic. As the pandemic recedes it is reasonable to assume this demand will resurface.
There are particular concerns around falling numbers of cancer referrals. Dr Richard Johnson of the Royal College of Surgeons told the Committee that “[t]here's a massive unmet need in the community where patients haven't come forward yet and haven't been diagnosed”. Macmillan Cancer Support estimate that between March and November 2020, around 3,500 people could have missed a cancer diagnosis.
A report from Community Health Councils in Wales looking at the experiences of patients on waiting lists during the pandemic, says that many people were reluctant to use health services, due partly to concerns around COVID-19 infection.
The impact of waiting on patients can be enormous. Not only must people on waiting lists live with their condition for longer, they may find it getting worse. The HSCS Committee heard that patients may need extra support or ‘prehabilitation’ before being able to begin treatment, and people referred by GPs may need a greater level of diagnostic support.
“The effect on patients waiting for surgery, even if it's just planned surgery, is quite devastating both from a physical and a psychological point of view”, according to the Royal College of Surgeons.
How will the NHS in Wales deal with the backlog?
The Chief Executive of NHS Wales has stressed that reducing waiting times needs major changes in patient care, “making sure that we don't just revert to our traditional services”. The Welsh NHS Confederation also acknowledge the need to “radically rethink” the way healthcare is delivered, including:
- Substantially increased use of digital technologies in providing accessible care. Greater use of virtual GP and out-patient consultations is perhaps the most significant service change which emerged during the pandemic;
- Supporting patients as partners in managing their own care, with access to better information and advice on their health;
- More team working across primary care and hospitals, including more and better organised support for people with chronic conditions;
- Increased support for GPs and primary care, such as more direct GP access to diagnostic services;
- Providing some services more regionally, with health boards working together in areas such as diagnostics and less complex, high-volume surgery.
What are the barriers to tackling waiting lists?
The Committee heard from health boards and professional bodies about issues that must be addressed in tackling the backlog. These include the continuing impact of the pandemic on service demand and capacity, with hospitals needing to separate COVID and non-COVID treatment. There's also a need for improved scaling up of innovation. The Wales Audit Office, alongside other evaluation work, has been critical of NHS Wales’ record in rolling out successful good practice;
Staff need time to recover and recuperate, there needs to be an increase in the workforce, and access to more service capacity, in both the NHS and independent sector. This will all need additional funding.
What could the new Welsh Government do?
The waiting times figures are daunting. The then Minister for Health and Social Services, Vaughan Gething, said on 24 February 2021 that he believed the recovery will take at least a full Senedd term.
These pressures aren’t unique to Wales. The Nuffield Trust report that waiting lists in England are at their highest point since August 2007, and the NHS Confederation estimates that NHS England faces a “hidden waiting list” of nearly six million people who haven’t used health services or been referred. Public Health Scotland reported that, in December 2020, almost 40% (34,456) of patients had waited over 39 weeks for treatment, with lengthy waiting times for out-patient appointments as well.
Recovering from the pandemic involves clearing the existing backlog, and keeping up with demand from new patients added to waiting lists. The previous Welsh Government recently published a recovery plan for health and social care. This proposed changes in outpatient services, with virtual appointments and direct GP access to tests becoming normal practice, to reduce referrals to hospital services. It also recognised the need for additional service capacity.
NHS activity remains constrained by COVID-19 restrictions and the need to retain capacity to deal with further outbreaks. Waiting times were increasing before the pandemic. Radical action may be required by the new Welsh Government if it wants current waiting lists not just to stabilise, but to shrink.
Article by Paul Worthington, Senedd Research, Welsh Parliament






