What is Antimicrobial Resistance?
Antimicrobial resistance (AMR) is a global public health issue that threatens the effectiveness of antibiotics and other antimicrobial medicines that have become essential staples of the modern medical arsenal. Over time, pathogens such as bacteria are able to evolve resistance to antimicrobial drugs – in the case of a bacterial infection this would mean reduced susceptibility to one or more antibiotics. When a particular pathogen is not susceptible to clinical treatments with these drugs, it is considered ‘resistant’ to the drug.
The Review on Antimicrobial Resistance (PDF 2.25MB), commissioned in 2014 by then Prime Minister David Cameron and chaired by economist Lord O’Neill of Gatley, made dire predictions about the consequences of AMR if it was not effectively responded to by policymakers:
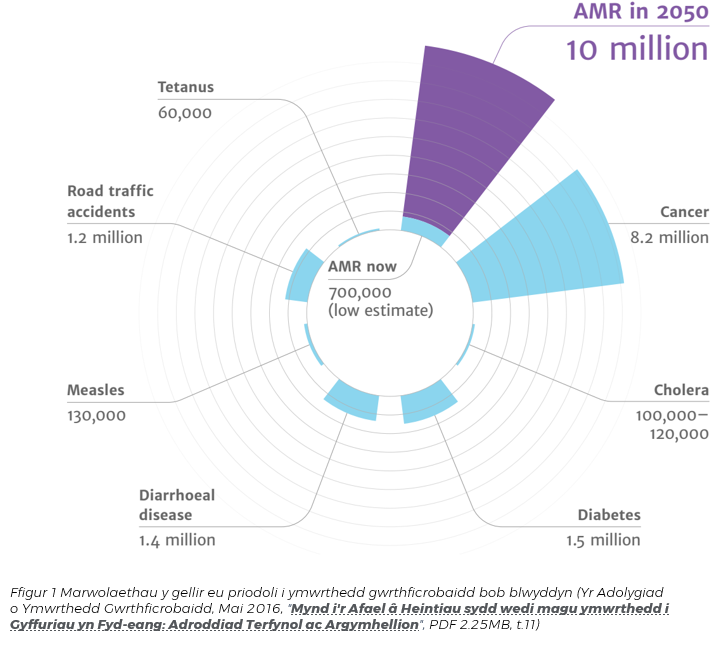
“We estimate that by 2050, 10 million lives a year and a cumulative 100 trillion USD of economic output are at risk due to the rise of drug resistant infections if we do not find proactive solutions now to slow down the rise of drug resistance. Even today, 700,000 people die of resistant infections every year. Antibiotics are a special category of antimicrobial drugs that underpin modern medicine as we know it: if they lose their effectiveness, key medical procedures (such as gut surgery, caesarean sections, joint replacements, and treatments that depress the immune system, such as chemotherapy for cancer) could become too dangerous to perform. Most of the direct and much of the indirect impact of AMR will fall on low and middle-income countries” (p. 4).
The World Bank (PDF 3.75MB) has warned that the impact of AMR “might cancel decades of progress in global economic convergence” (p. 18), with the economic cost of AMR varying across country income groups.
Public Health Wales (PDF 3.62MB) has identified AMR as an “increasing problem in Wales [that] has already led to a small number of difficult to treat infections, leading to failed therapy and potential complications” (p. 3).
World Antibiotic Awareness Week
World Antibiotic Awareness Week has been held every November since 2015. The initiative is led by the World Health Organisation (WHO) as part of its objective to “improve awareness and understanding of antimicrobial resistance” – one of the five strategic objectives from the WHO’s Global Action Plan (PDF 235KB). Previous themes have been “Antibiotics: Handle with Care” (2015 and 2016) and “Seek advice from a qualified healthcare professional before taking antibiotics” (2017). In 2018, the key messages are “Think Twice, Seek Advice” and “Misuse of Antibiotics puts us all at Risk”, though there are also five “focus” days of tailored messaging around each of the Global Action Plan objectives.
Antimicrobial Resistance in Wales
The Welsh Government’s delivery plan for AMR covering 2016-2018, “Together for Health: Tackling Antimicrobial Resistance and Improving Antibiotic Prescribing” (PDF 756KB), was released in March 2016 with seven delivery themes:
- Improving infection prevention and control practices
- Optimising prescribing practice
- Improving professional education, training and public engagement
- Developing new drugs, treatments and diagnostics
- Better identification and prioritisation of AMR research needs
- Better access to and use of surveillance data
- Strengthened international collaboration
The plan focuses primarily on human health, because the control of veterinary use and prescribing of antimicrobials is not devolved to the Welsh Government.
In May 2018, the Welsh Government introduced improvement goals (PDF 589KB) for antimicrobial prescribing for the 2018-19 financial year. The goal for both primary care and secondary care is a 5 percent reduction against the baseline year of April 2016 – March 2017.
A Public Health Wales report, “Antibacterial Usage in Primary Care In Wales 2013/14-2017/18” (PDF 7.11MB), published on 1 August 2018 presents the recent progress in reducing antibacterial use in GP Practice in Wales. The report observed an 11.9 percent reduction in total antibacterials dispensed across the GP practices in Wales over a five year period from the 2013/14 financial year to 2017/18. In 2017/18, the total volume of antibacterial items dispensed for GP practices in Wales showed a 2 percent reduction in usage compared with the 2016/17 financial year.
In 2017/18, there was a reduction in total antibacterial usage in six of the seven Health Boards, most notably in Betsi Cadwaladr University Health Board with a 5.9 percent reduction. Cwm Taf University Health Board had a 0.8 percent increase.
The report also notes a significant variability between GP Clusters in gross annual antimicrobial use in 2017/18, with a 36 percent difference in prescribing rates between the GP Cluster with highest annual rate (South Rhondda) of dispensed items and the GP Cluster (North Ceredigion) with the lowest rate.
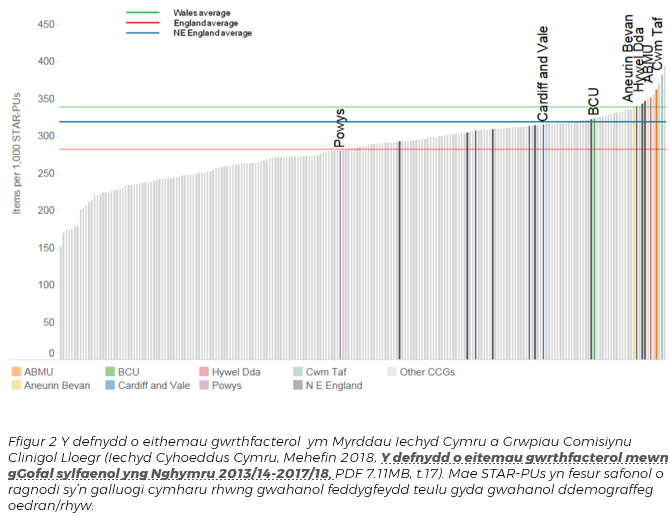
As Figure 2 illustrates, the average rate of dispensed antibacterials for Wales is currently higher than England (and the North-East of England, which is demographically similar to Wales). Most of the seven Health Boards in Wales are among the highest dispensers when included with English Clinical Commissioning Groups.
A further report published on 1 June 2018 by Public Health Wales, “Antibacterial Resistance In Wales 2008-2017” (PDF 3.62MB), observed that there had been an increase in antibacterial resistance among the three most common bacterial causes of bloodstream infections in Wales in 2017. In an NHS Wales news item in August 2018, Eleri Davies, a co-author on the report, stated that “antibacterial resistance in Wales is comparable to the aggregated rates and trends for the UK. However, there is considerable variability between areas and hospitals.”
The Chief Medical Officer for England, Professor Dame Sally Davies, highlighted in her 2013 book The Drugs Don’t Work: A Global Threat that an ageing society with an increased number of patients with comorbidities may lead to higher antibiotic prescribing rates than would be necessary in younger and healthier societies. A report (PDF 989KB) published in October 2018 by the National Assembly for Wales Finance Committee, following its inquiry into the cost of caring for an ageing population, states that witnesses had “noted a sharp and significant increase in demand across health and social care, in part because of the higher levels of care and support required by people , the complex nature of the support required and the presence of a number of additional health issues co-occurring with a primary one (or “comorbidity”)” (p.18). The report additionally notes that the Office for National Statistics has projected that the proportion of older people in Wales, which has been increasing over the last decade, will continue to increase in future years.
Article by Alistair Anderson, National Assembly for Wales Research Service The Research Service acknowledges the parliamentary fellowship provided to Alistair Anderson by the Economic and Social Research Council, which enabled this Research Briefing to be completed.