Article by Paul Worthington, National Assembly for Wales Research Service
This article is taken from ‘Key issues for the Fifth Assembly’, published on 12 May 2016.
Proposals for changing hospital services have proved controversial. What is the case for and against change, and how will the new Welsh Government respond?
Proposed change to hospital services is almost certain to arouse intense scrutiny. Communities feel strongly about their local hospitals. Service reconfiguration has become a loaded term and opinions can easily become polarised. For some, changes are seen as a threat of ‘down-grading’ services; others may see them positively and as essential improvement. The previous Welsh Government consistently identified the need for change in Welsh health services, shifting investment and services from hospitals into the community. The Wales Audit Office, the British Medical Association (BMA) and the Welsh NHS Confederation have echoed that call, arguing that radical transformation of healthcare is essential to ensure the long term sustainability of NHS Wales. There is also a professional consensus that some specialist hospital services are too thinly spread, leading to concerns about the training and recruitment of doctors. The Welsh NHS Confederation, the BMA and health policy commentators have stressed the need for honest conversations with the public and clinicians about service choices and how those choices will impact on local healthcare services. Patients, the public and some clinicians have expressed doubts about the rationale for change and voiced concerns about how effectively proposals are discussed with the people and communities who will be affected.
What is the case for change?
In 2012, the Welsh Institute for Health and Social Care (WIHSC) published an independent review on the configuration of Welsh hospital services. This review contained several key conclusions:
- the existing configuration of hospital services was not delivering the best outcomes for patients;
- medical staff shortages could lead to unplanned closure and possible collapse in some services;
- increasing specialisation means that centralising expert clinical staff and concentrating certain services onto one site could deliver better patient outcomes in some services;
- centralisation could mean longer travelling distances, but the impact can be reduced by boosting care outside hospital and better transport; and
- the case was strong for changing how some hospital services are provided.
The Bevan Commission has also published an influential paper on Prudent Healthcare (2013), which identified a pressing need for delivering more healthcare outside hospital, and the previous Welsh Government explicitly accepted the Prudent Healthcare recommendations as a basis for action. The case for change has not been universally accepted. Opposition parties, pressure groups, local communities and some clinicians have expressed doubts. There have been calls for a moratorium on hospital closures and the re-opening of some hospital and minor injuries services. Work by the Kings Fund in England has supported the case for service change, but also counselled caution about its impact, emphasizing that there is no single solution for local services. Change is not always inevitable. Proposals for centralising maternity services in north Wales were challenged by local communities and clinical staff. Betsi Cadwaladr University Health Board subsequently decided not to proceed with the proposals.
What are the challenges?
Alongside calls for shifts from hospital care, demand on acute hospitals across Wales continues to rise, with high levels of A&E attendances and emergency admissions. The main users of acute NHS services are aged over 65, and in Wales we have a growing number of older people. The Chief Medical Officer has argued that acute hospitals are not necessarily the ‘right place’ for older people, but notes they are likely to stay longer in hospital, partly because of rehabilitation needs. Wales also has increasing levels of chronic disease including diabetes, joint problems and heart disease, which will increase demands on health services. Much of the evidence argues that managing this demand requires investment in stronger primary and community care.
What has happened so far?
Wales has 16 major acute hospitals, and over 50 community hospitals – excluding mental health and specialist cancer provision.
Major acute hospitals in Wales
There has already been change. Some community hospitals and minor injury units have closed, although new services have opened in the Cynon Valley, Ystrad Mynach, Builth Wells, Flint and 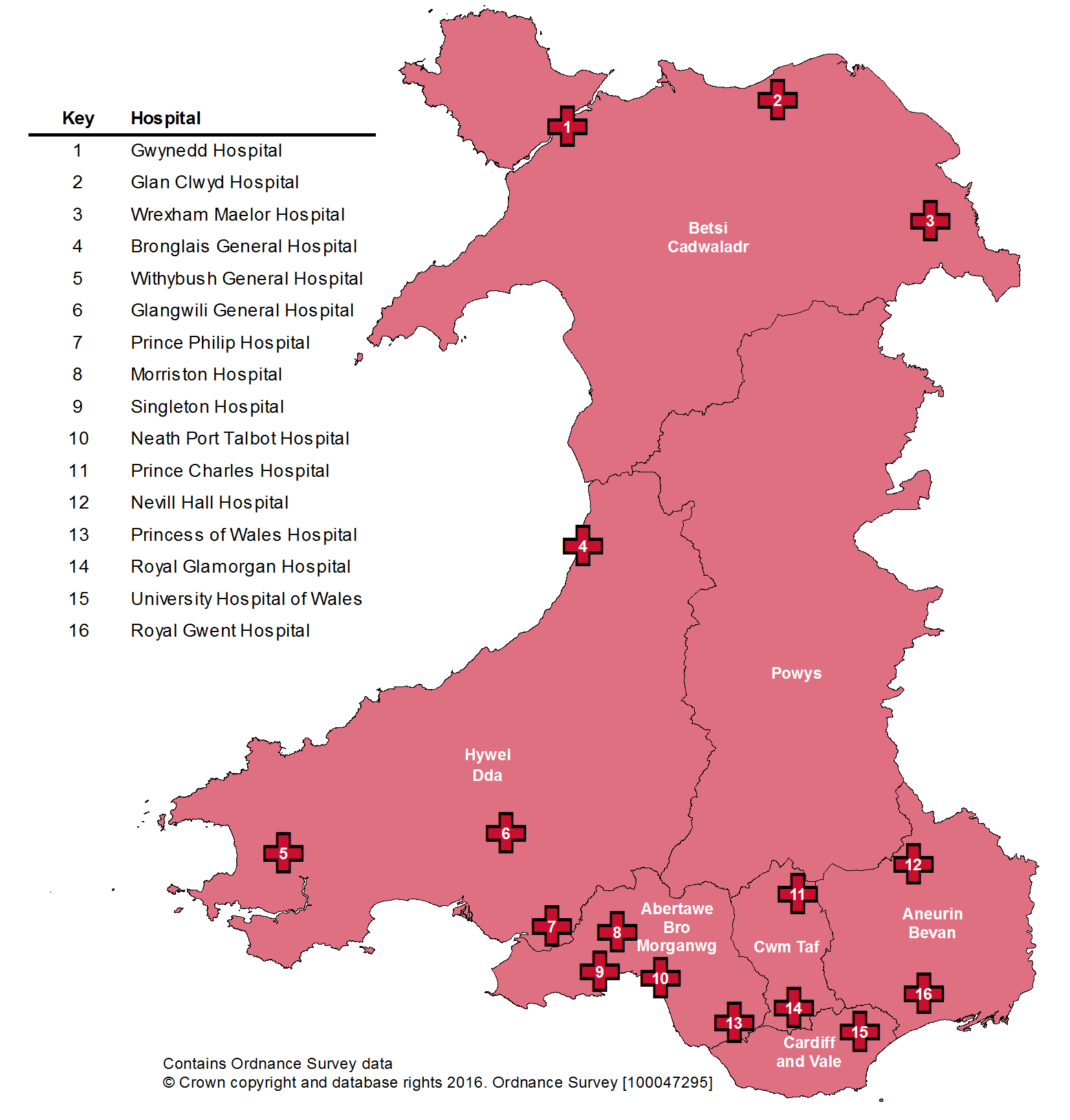 elsewhere. The previous Welsh Government focused much additional investment in primary and community care services rather than in hospitals. There have been major consultations on reconfiguring hospital services in north, west and south Wales and change is already happening in major acute hospitals, including:
elsewhere. The previous Welsh Government focused much additional investment in primary and community care services rather than in hospitals. There have been major consultations on reconfiguring hospital services in north, west and south Wales and change is already happening in major acute hospitals, including:
- maternity services moving from Withybush Hospital, Haverfordwest to Glangwili Hospital, Carmarthen;
- new GP and nurse-led emergency care services opening at Prince Phillip Hospital, Llanelli;
- changes beginning in A&E, maternity, paediatrics and neonatal care, which will be provided in fewer hospitals across south Wales; and
- stroke assessment services centralising onto one site in Cwm Taf.
Health boards are working on proposals about the future of other services, including major trauma, diagnostics and some surgical specialties: the outcome may be calls for enhanced community support but centralising more hospital services. However, there is little published on this front at present. Debate about the future of Welsh healthcare is unlikely to disappear. How will the new Welsh Government respond to the different views, pressures and choices that will determine the direction and sustainability of health services in Wales?
Key sources
- Bevan Commission, Simply Prudent Healthcare (2013)
- Wales Audit Office, NHS Wales: Overview of Financial and Service Performance 2013-14 (2014)
- Welsh NHS Confederation, The 2016 Challenge A vision for NHS Wales (PDF 624KB) (2015)
- WIHSC, Best configuration of hospital services for Wales: A Review of the evidence (PDF 953KB) (2012)