As we head for our third winter with COVID-19, we’re past the pandemic stage and total cases continue to fall. But concerns remain about pressures on health and social care services, and long COVID.. The Minister for Health and Social Services has warned we could experience spikes in both COVID-19 and flu over the coming months.
This article looks at the current position; the numbers of cases, the trends in those numbers, and some of the potential challenges over the coming months.
COVID-19 infections
The Chief Medical Officer (CMO), Sir Frank Atherton, recently told the Senedd’s Health and Social Care Committee that “the rates really have come crashing down” but warned we weren’t yet “out of the woods”
Data published by Welsh Government from the Office for National Statistics (ONS) indicates that the trend in people testing positive for COVID-19 in Wales continued to decrease since the beginning of the year, but has seen some increase in September (latest available data).
Chart 1: Official estimates of the percentage of the population in Wales testing positive for COVID-19 on ear nose and throat swabs since 10 August 2022
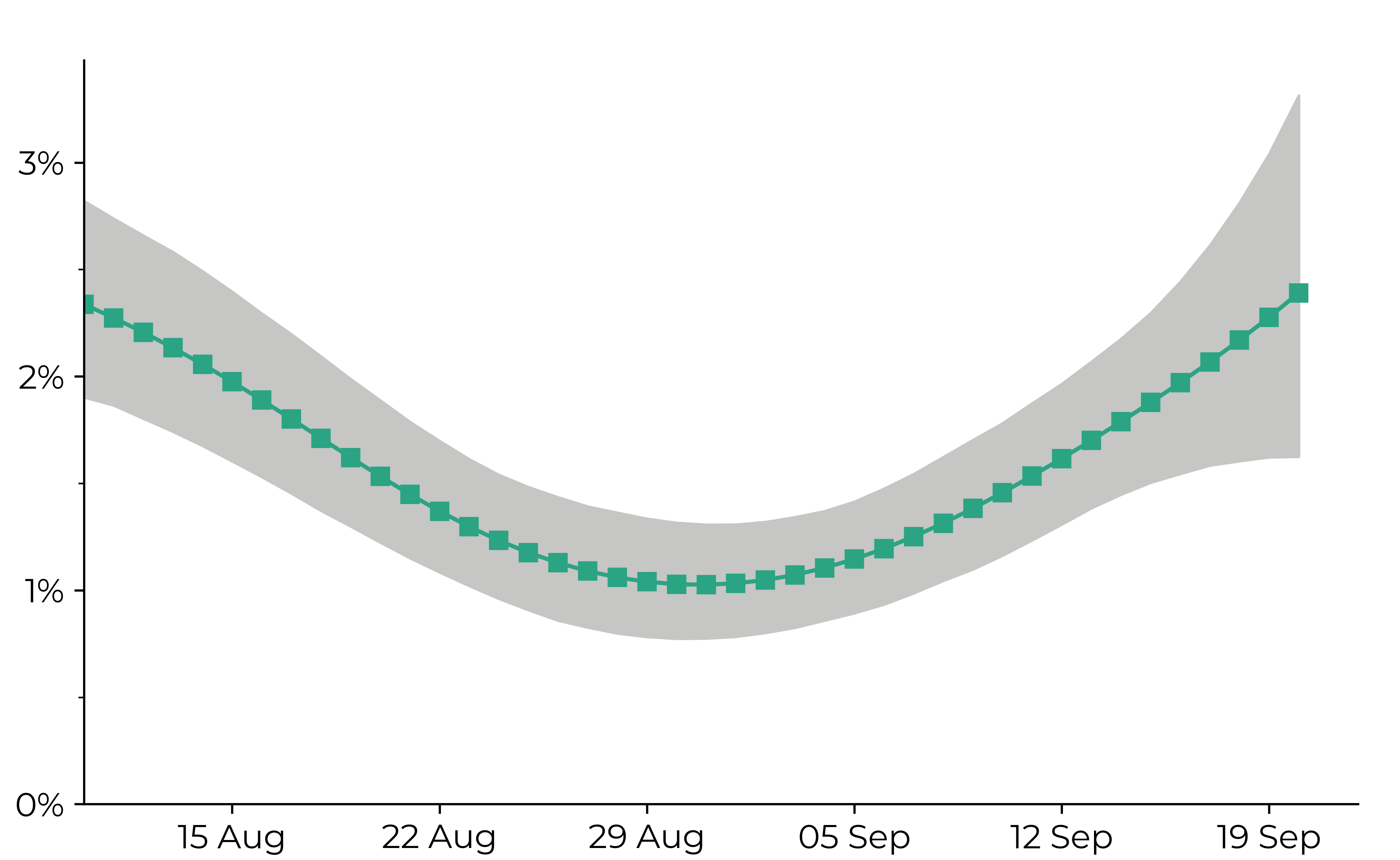
Source: ONS COVID-19 Infection survey. The green line and shading represent the modelled trend and 95% credible intervals based on the latest data.
The Welsh Government notes that the estimates are based on a relatively low number of positive tests, so we should be cautious about over-interpreting any small movements in the latest trend. We also don’t have the same level of totality around figures as when there was mass testing.
Chart 2: Official estimates of the percentage of the population in the UK countries testing positive for COVID-19 on ear nose and throat swabs since 10 August 2022
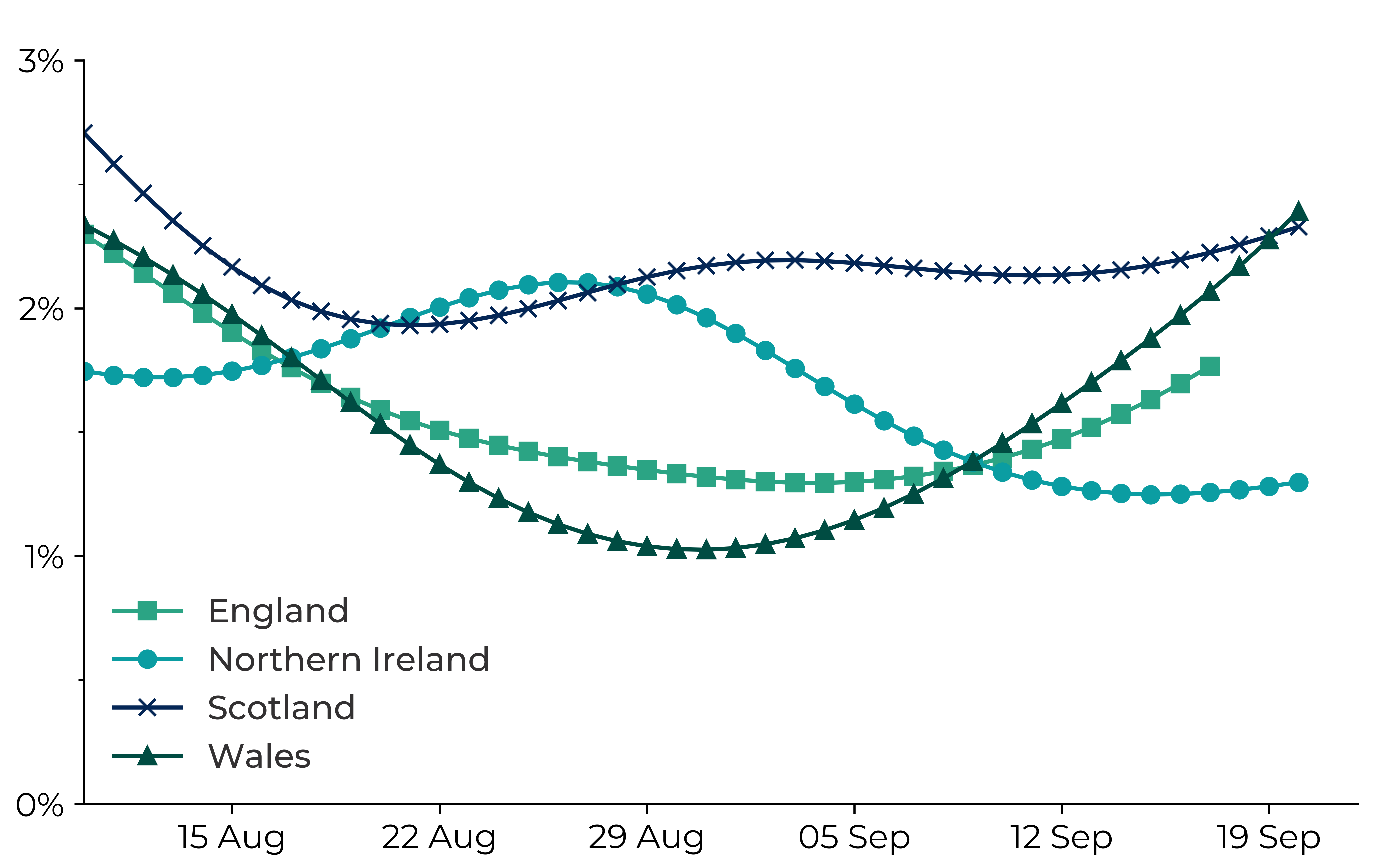
Source: ONS COVID-19 Infection survey. The lines represent the modelled trends based on the latest statistics.
The chart above shows that the estimated percentage of people living in private households testing positive has decreased overall since the beginning of the year although there has been some increase during September. The most recent estimated figures indicate:
- Wales: 62,900 – around 2.07% or 1 in 50 of the population;
- England: 857,400 - around 1.57% or 1 in 65 of the population;
- Northern Ireland: 23,100 - around 1.26% or 1 in 80 of the population; and
- Scotland: 117,100 - around 2.22% or 1 in 45 of the population.
This overall downward trend in UK infections mirrors the pattern globally as reported by the World Health Organisation.
COVID-19 deaths
ONS data shows COVID-19 mortality rate for Wales decreased to 29.6 deaths per 100,000 people in August 2022, compared to 36.1 deaths per 100,000 in July and 72.2 per 100,000 in January.
The rates in England decreased to 30.5 deaths per 100,000 in August 2022 compared to 32.6per 100,000 in July and 79.3 per 100,000 in January.
COVID-19 was the seventh leading cause of death in Wales (3.0% of all deaths) in August and the sixth in England (3.3% of all deaths), but the mortality rates are significantly lower than at the peaks of the pandemic.
COVID-19 variants
Since the end of June, the majority of UK COVID-19 infections have been Omicron variants BA.4 or BA.5, with BA.5 comprising 86.3% and BA.4 comprising 12.2% of all sequenced COVID-19 infections in the week ending 14 August. PHW publish weekly data on variants of concern and variants under investigation for Wales
Long COVID
Long COVID is when symptoms continue, or new symptoms develop, more than 12 weeks after infection with COVID-19. It’s still not clear about how many are affected; the WHO indicate long COVID affects about 10% of people, but the Chief Scientific Adviser for Health, Dr Rob Orford, says the figure for Wales may be around 8%.
The ONS estimates 2 million people in UK private households (3.1% of the population) were experiencing self-reported long COVID as of 31 July. The estimate for Wales was 90,000, slightly down from May and June, with around 2,500 people being referred into long COVID support services in Wales.
Impact on health and social care services
An average of 15 people a day were admitted to hospital in Wales with confirmed or suspected COVID-19 in the week ending 11 August, compared to the average of 16 for the week to 2 August. This is a significant reduction from admissions at the peaks of the pandemic, as shown in the chart below.
However, pressure on services is evident, with general and acute medical bed occupancy in acute hospitals at 94.6% as at 27 September. The Minister recently said :
While we are currently in a stable position, we know that seasonal flu and COVID-19 viruses have the potential to add substantially to the winter pressures faced by the NHS, particularly if infection waves from both viruses coincide.
The CMO has also acknowledged that pressure on services is “much more extreme than we've seen at this time of the year in any previous years”.
Chart 3: Patients admitted to hospital as suspected or confirmed with COVID-19, from 1 April 2020
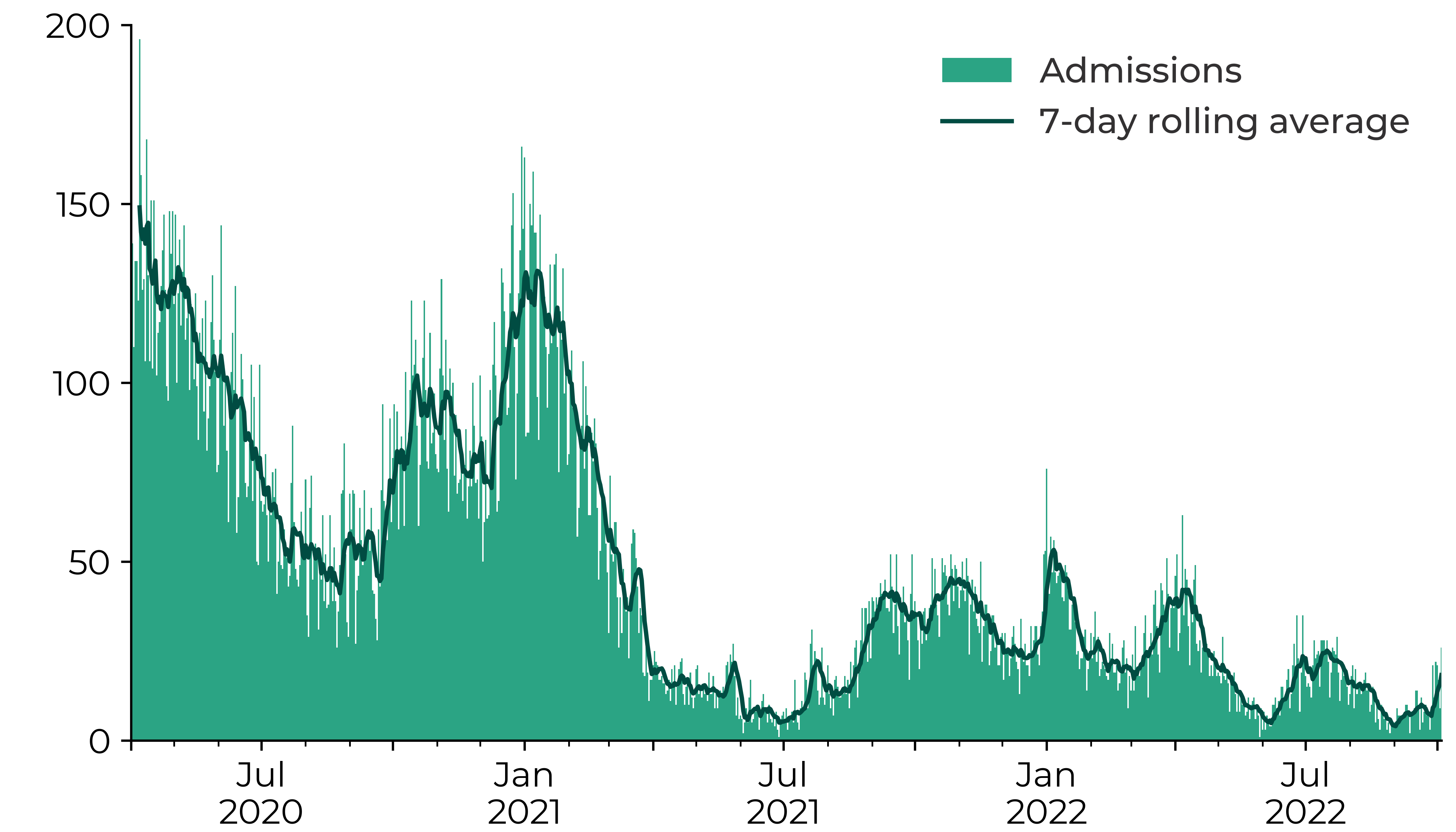
Source: StatsWales
Looking at NHS staff absence data, 0.6% of NHS staff - about 600 - were absent due to COVID-related sickness in the week ending 22 August. Another 0.4% of staff were having to self-isolate. Average total absence stands at 5.7% compared to a usual pre-pandemic figure of about 5%.
COVID- 19 vaccination programme
The Welsh Government’s Winter respiratory vaccination strategy: autumn and winter 2022 to 2023. states:
We must learn to live with endemic coronavirus, in the way we have been living with flu for many years.[….] Ensuring as many eligible people as possible come forward for both their flu and COVID-19 vaccinations will be critical to protect individuals, communities and our health and care services this winter.(p.4)
Speaking to the Health and Social Care Committee, the CMO advised that:
…having your vaccine, if it's offered, is the best available defence—you're far less likely to end up in hospital than if you don't get your booster jab.
Whilst acknowledging the vaccine effectiveness does wane over time, he stated “the reduction in harm, in serious harm, seems to be maintained”.
The roll-out of the COVID-19 autumn booster started on 31 August. This includes residents and staff working in care homes, frontline health and social care workers, those aged 50 and over, and those aged 5 to 49 years in clinical risk groups.
Public health issues and prevention
There are global echoes of the warnings about the coming winter. The European Centre for Disease Prevention and Control has set out concerns about possible new waves of transmission as a result of new variants and waning vaccine immunity.
The WHO has launched an autumn/winter strategy for COVID-19 and other respiratory viruses which “calls on countries to relaunch mitigation efforts” alongside vaccination. This includes promoting mask-wearing indoors and on public transportation, ventilating crowded and public spaces, and handwashing.
The British Medical Association has expressed concerns about the removal of key public health measures, such as free testing, self-isolation support payments, and the limited dissemination of public health messaging.
The ONS has noted that the proportion of people taking preventative measures or feeling worried about COVID-19 has been decreasing since spring 2022. It reports the proportion of people wearing face coverings has dropped from 65% in the spring, to 35% in the latest period.
Note: Public Health Wales (PHW) publish a range of data relating to COVID-19, including information on vaccinations, mortality, variants, hospitalisation, hospital-acquired infections, and testing.
Article by Paul Worthington, Senedd Research, Welsh Parliament






